
Here is a summary of various programming projects that I have worked on while at Bangor University (2013-2015) and the University of Chester (2015-2017).
1. Image Projection onto Patients (IPoP)
Edwards, Marc R., et al. "Real-Time Guidance and Anatomical Information by Image Projection onto Patients." Eurographics Workshop on Visual Computing for Biology and Medicine. Eurographics Association, 2016.
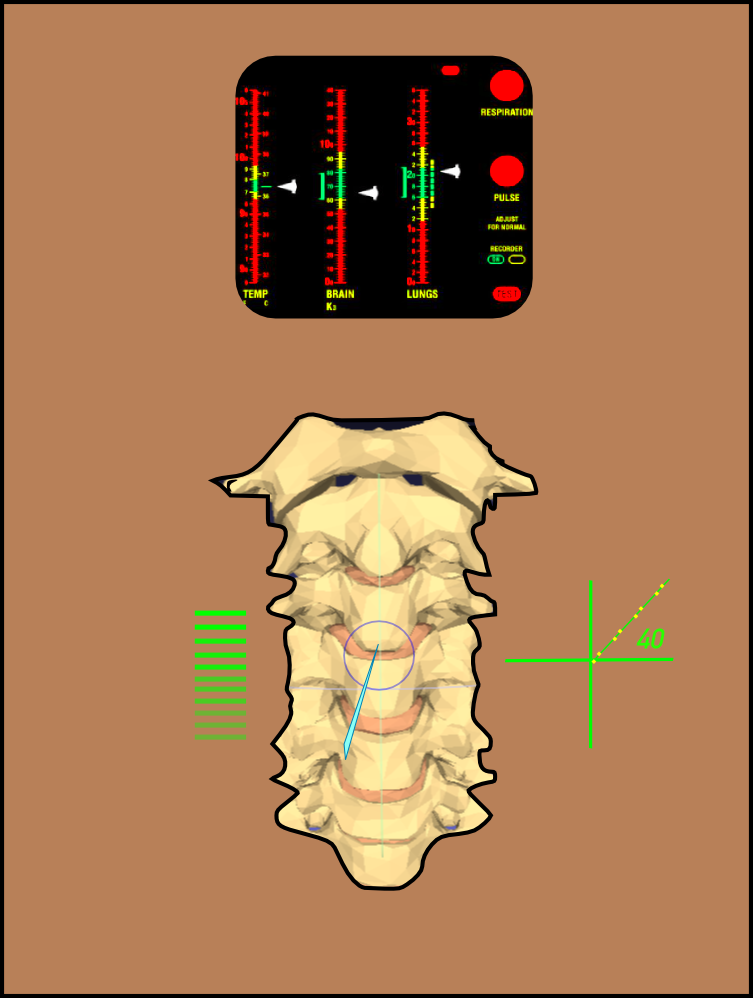


Projecting anatomical data onto patients to visualise what is directly under the skin could help improve surgical performance and patient comfort. This technology could greatly help lumbar puncture which normally requires the doctor to feel the correct puncture location and angle on the spine.
Areas that I covered include; patient tracking, image projection and colour adjustment, to achieve best contrast on various skin colours. Tracking methods included the use of infrared reflective markers, Kinect and a 6DOF motion tracker composed of a gyroscope and accelerometer, used to track the needle and patient.
This video shows preliminary work towards the solution. Tracking was done using the following technologies: Python, TKinter, OpenCV and reflective markers.
Subsequent versions were built using Java and C++ programming languages as we needed to use multithereadig to increase software performance.
2. Cost effective axial force sensor
A report on this device is attached here.
Imagine for a moment that you are performing a needle puncture. How could you tell that you have arrived at the correct tissue depth? You can approximate using needle displacement, but what if you could also visualise the needle force profile into tissue layers?
Force sensors when attached to biopsy needles can be used to identify layers from the puncture force profile. As the needle traverses various tissue layers the change in tissue density is detected. I developed a low cost force sensor rig that can be easily used with the needle to measure axial needle forces.


To test this concept, a basic sensor glove was built from a force sensitive resistor (FSR) and an Arduino micro-controller programmed to measure needle force. The FSR was attached to the thumb of the glove (to achieve better covering of the FSR) which was used to push the biopsy needle into tissue samples.
Testing was done using lambs liver and a training lumbar medical phantom. Results suggested little hysteresis associated with the FSR and similar force profiles to published data, though absolute force values differ.

PROBLEM: requires constant velocity of needle puncture.
SOLUTION 1: Robotic puncture rig
SOLUTION 2: Realtime mapping of force measurements with needle acceleration.
3. Blood flow analysis in an aneurysm simulator


Nylon particles. Greatest blur at highest flow.

Blood flow modelling is useful for identifying potential regions for aneurysms in circulatory systems. A blood flow model, developed in collaboration with Bangor and Liverpool universities, was filled with nylon coated particles in a fluid. Flooding this system with red laser light better revealed the moving particles for image processing methods.
My challenge was to come up with a way of measuring the flow of these particles (relative velocity within the model). My solution was to segment the particles from each video frame and measure their elongation, due to image blurring, using image processing. Greatest elongation particle images occured at greatest flow velocity. From this information, the relative speeds of particles was approximated from the known fluid flow velocity.

4. Stent dilation pressure-volume measurements

Stents are used to dilate blood vessels and to increase blood flow. There is a lack of research into the relationship between pressure of the stent and the shape it adopts in the blood vessel. Bangor university has a stent pressure monitor but there was no way of measuring the volume of the stent during dilation.
I developed a computer vision method for approximating the volume of the stent during dilation by illuminating it with light to maximise contrast, and assuming that the stent takes on a spheroidal shape. Measuring stent volume was done indirectly by placing it in water containing a water level sensor used measures the change in water volume as the stent dilates. I also built various wooden rigs to simulate various blood vessel shapes.
This method was used as part of a third year undergraduate computer science project in collaboration with a medical consultant heart surgeon.
PROBLEM: The stent shape becomes non-spheroidal as it approaches maximum pressure in constricted environments.
5. Towards a cost effective haptic device
A report on this device is attached here.




The high cost of commercial haptic devices used for
needle puncture simulations prompted the development of a low cost alternative. A colleague of mine (C. Hughes) invented the use of a motorised sliding potentiometer as a cheap and programmable haptic device when connected to a micro-controller. I developed another version with a more powerful motor with a 3D printed holder as well as a method for testing its effectiveness as a haptic device. Testing was done by measuring the output force and comparing it to the expected programmed force profile using the FSR sensor above.
Though the device is cheap to buy, easily programmable and customisable, it requires further development in order to reduce the transformations in forces due to friction and vibration of the mechanical components.
6. Computer vision based prototype for biopspy simulator.
During my development of a prostate biopsy simulator at Bangor University I developed a computer vision method for tracking which grid coordinate of the needle guide is used. This was an important step towards the recording of grid holes as part of the biopsy simulator.
The method you see here overlays a matrix of circles over the biopsy guide holes. The pixel values within these circles are checked and anything above a threshold brightness is identified as a needle tip. In the video I simulate a needle tip using laser.
7. Biopsy Simulator
P. D. Ritsos, M. R. Edwards, I. S. Shergill, and N. W. John, “A Haptics-enabled Simulator for Transperineal Ultrasound-Guided Biopsy,” in Eurographics Workshop on Visual Computing for Biology and Medicine, 2015.

